Prostate
|
Purpose
|
Detect and differentiate clinically significant prostate cancer from benign diseases and dormant malignancies.
|
Patient preparation
|
- If examination is being performed for staging, an interval of at least 6 weeks or longer between prostate biopsy and MRI should be considered.
- The patient should use the rest room (seated) prior to the examination to evacuate the bladder and rectum.
- An endorectal coil is no longer typically used.
|
Radiologist should know
|
- Recent serum prostate-specific antigen (PSA) level and PSA history
- Date and results of prostate biopsy, including Gleason scores of positive biopsies
|
Sequences
|
Scout localizer images:
|
3 planes, 5 images. FLASH (spoiled GRE)
|
T2-weighted Axial Pelvis
|
Acquired from the iliac crest to pubic symphysis for overview evaluation of the pelvic soft tissues, in particular, to assess pelvic lymph nodes.
|
High Resolution T2 weighted
|
3 planes: Sagittal, Axial, Coronal. Acquired for measurement of prostate gland volume, detailed evaluation of prostate lesions and for evaluation of extracapsular involvement.
|
T2-weighted Space (3D)
|
Adjunct to 2D acquisition. Can be useful for distinguishing partial volume averaging effects from true lesions.
|
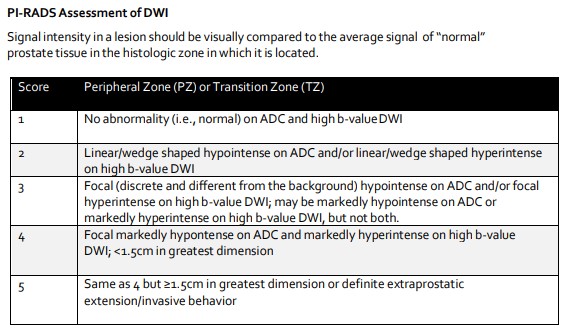
DWI with calculated ADC map
|
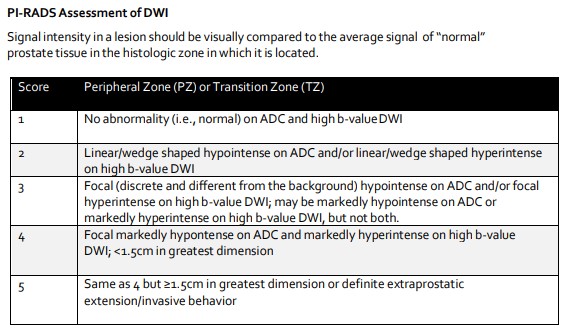
This is a key component of prostate imaging and needs to include an ADC map and high b-value images. Most clinically significant prostate cancers have restricted diffusion compared to normal tissue and appear hypointense on ADC maps. While there is a lot of overlap, ADC values have been reported to inversely correlate with histological grade. Similarly, on high b-value images clinically significant cancers will likely have preservation of signal because of restricted diffusion. High b-value images may be acquired or calculated by extrapolation from lower b-value acquisitions.
|
Axial T1-weighted MASK
|
VIBE, no fat saturation. Evaluation of this sequence provides information regarding hemorrhage within the prostate gland and provides a pre-contrast comparison for the post-gadolinium larger field of view images. Hemorrhage is typically hyperintense on T1-weighted images and hypointense on T2-weighted images; however, chronic blood products may appear hypointense on all sequences.
|
Axial T1-weighted dynamic contrast enhanced (DCE) images
|
Dynamic contrast enhancement provides information regarding the enhancement kinetics of lesions.
|
T1-weighted axial pelvis
|
Fat saturated post contrast larger field of view image allows for evaluation of extraprostatic tissue and bones.
|
|
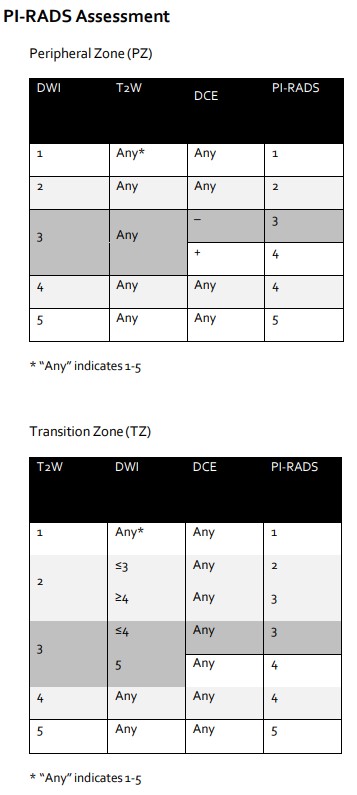
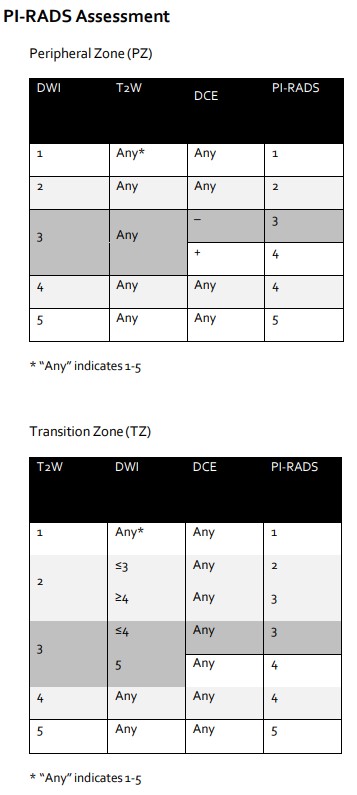
| PI-RADS 2 From ACR PI-RADS v2.1; see recommended reading
|
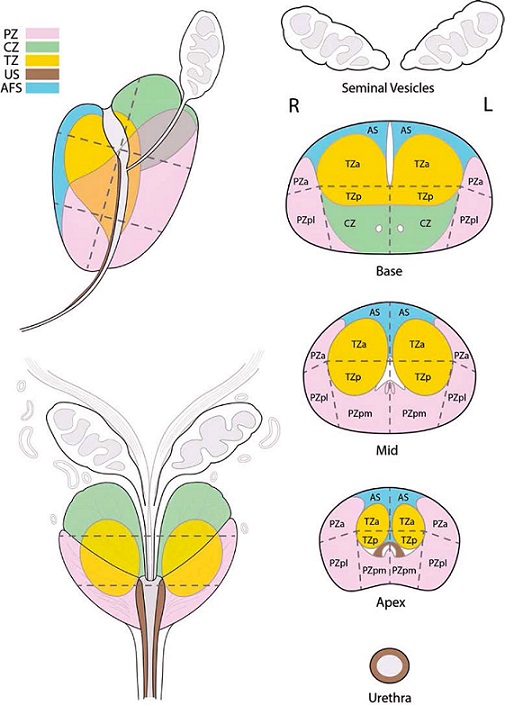
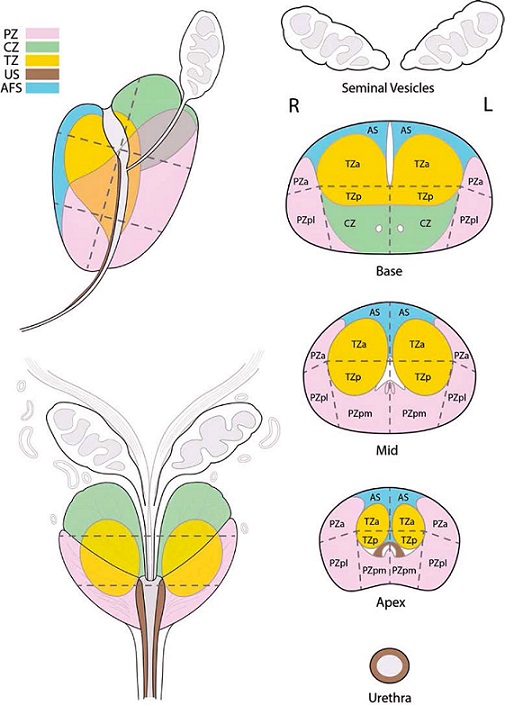
Note regarding interpretation: Prostate cancer is usually multifocal. Per PI-RADS v2.1, lesions with an assessment category of 3-5 should be assigned a Sector Map location and the dominant (Index) lesion should be specified. If there are more than four suspicious findings, typically only the four with the highest likelihood of clinically significant cancer (highest PI-RADS assesment category) should be reported per PI-RADS v2.1 guidelines. If two lesions have identical PI-RADS category, the dominant lesion would be the lesion with extraprostatic extension, even if it is not the largest.
OVERALL PI-RADS v2.1 Assessment Categories:
- PIRADS 1 — Very low (clinically significant cancer is highly unlikely to be present)
- PIRADS 2 — Low (clinically significant cancer is unlikely to be present)
- PIRADS 3 — Intermediate (the presence of clinically significant cancer is equivocal)
- PIRADS 4 — High (clinically significant cancer is likely to be present)
- PIRADS 5 — Very high (clinically significant cancer is highly likely to be present)
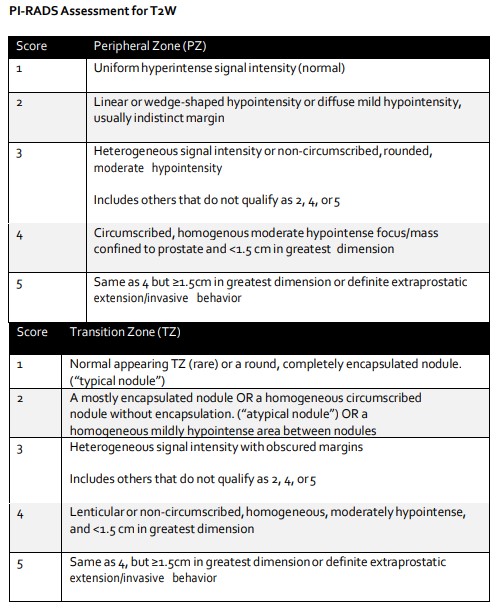
PI-RADS Assessment for T2W:
|
*For the transitional zone (TZ), T2-weighted images are the primary determining sequence. Approximately 20-30% of prostate cancers originate in the TZ.
|
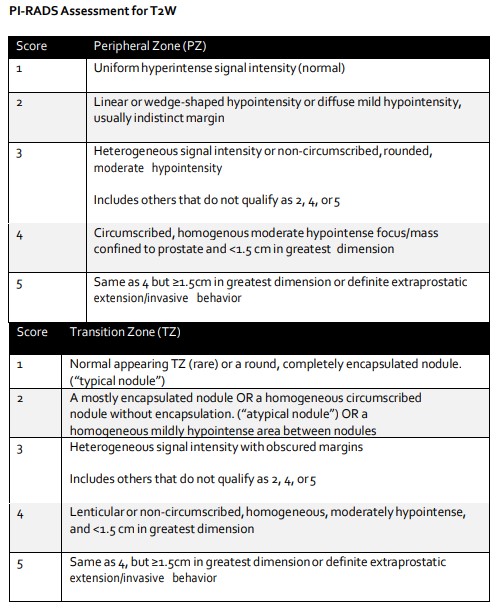
PI-RADS Assessment of DWI:
|
*For the peripheral zone (PZ), DWI is the primary determining sequence. Approximately 70-75% of prostate cancers originate in the PZ.
|
Prostate Sector Map from ACR PI-RADS 2.1:
|
Illustrative cases
|
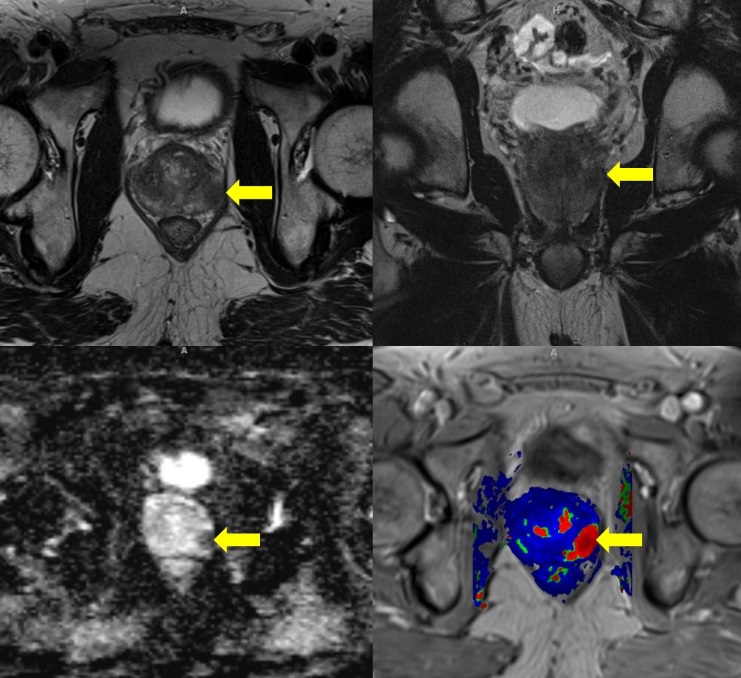
Case 1: GLEASON 4+3=7 ADENOCARCINOMA
with focal extraprostatic extension left posterior base
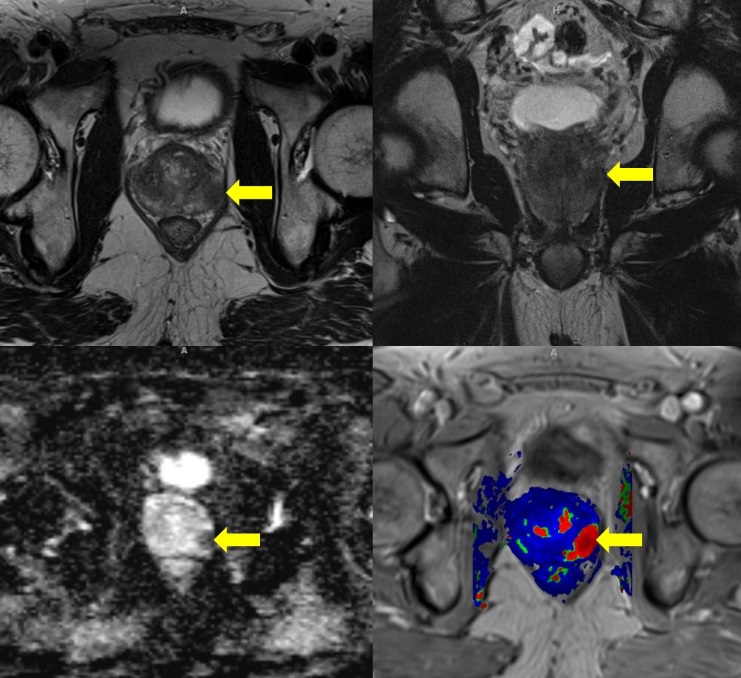
- Axial (upper left) and Coronal (upper right) T2-weighted high resolution sequences demonstrate a hypointense, dominant lesion in the left mid to base (PZpl) measuring up to 15 mm with extraprostatic extension (T2W assessment PI-RADS 5). ADC map (lower left) image with focal hypointensity measuring 15 mm (DWI assessment PI-RADS 5). DCE color-map image (lower right) with red color indicating focal early enhancement of the lesion (+ DCE).
- Pathology confirmed that the dominant nodule was Gleason 4+3 =7 with focal extraprostatic extension.
|
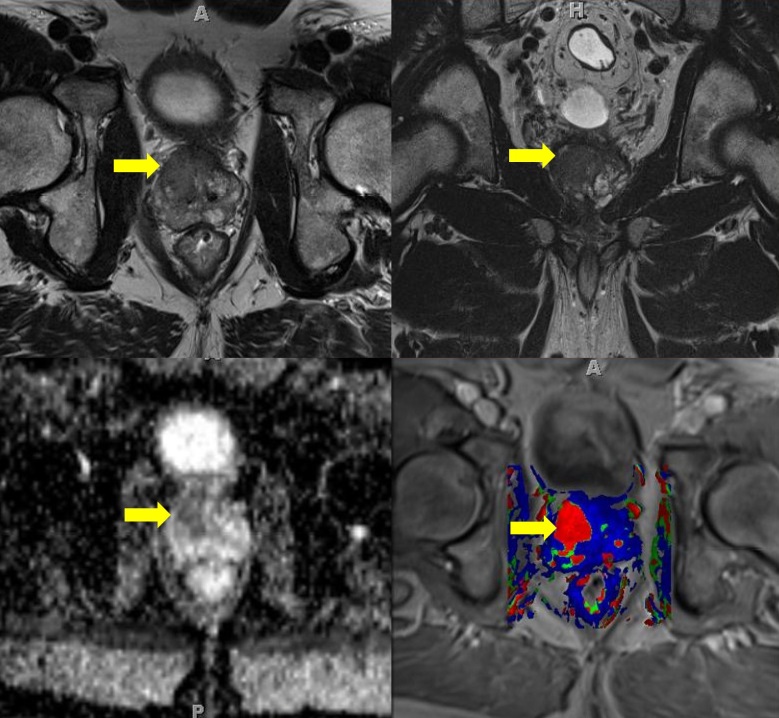
Case 2: GLEASON 4+3=7 ADENOCARCINOMA
with perineural invasion identified
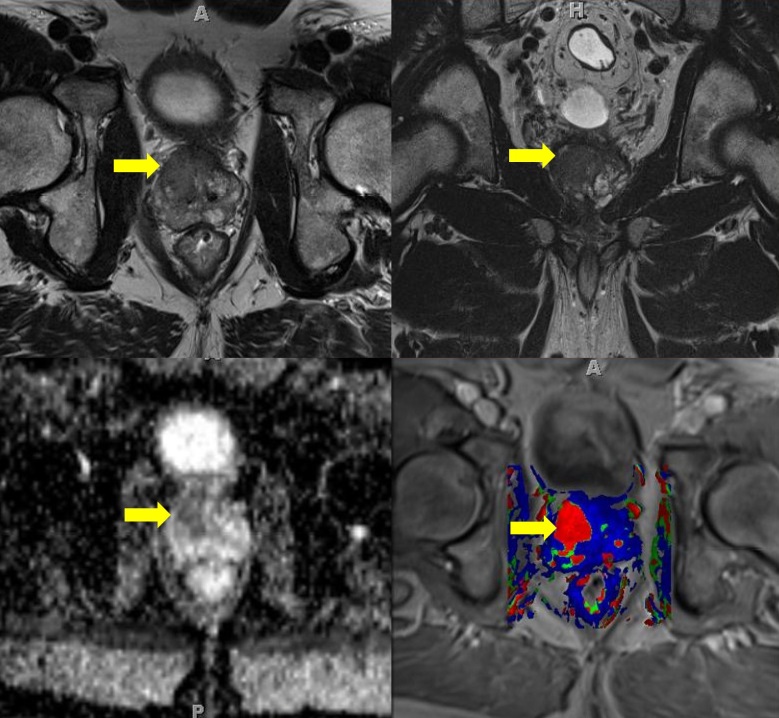
- Axial (top left) and Coronal (top right) T2-weighted high resolution sequences demonstrate a hypointense, dominant lesion in the right mid central gland (TZa) measuring up to 16 mm (T2W assessment PI-RADS 5). ADC map (lower left) image with corresponding focal hypointensity measuring 16 mm (DWI assessment PI-RADS 5). DCE color-map image (lower right) with red color indicating focal early enhancement of the lesion (+ DCE).
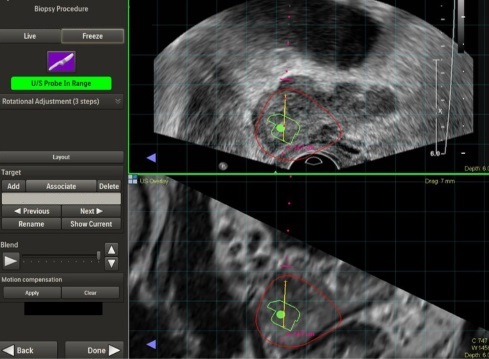
- Screen capture from UroNav MRI-US fusion biopsy (below) of targeted lesion in the right mid central gland.
- Pathology confirmed that the targeted lesion was Gleason 4+3 =7 with perineural invasion identified.
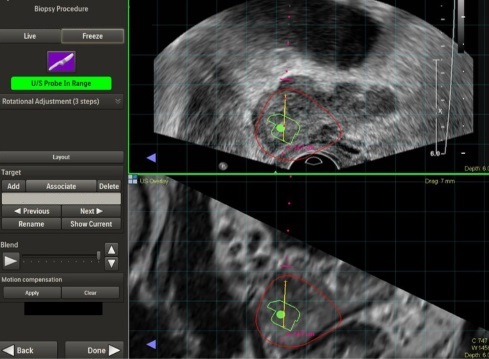
|
|
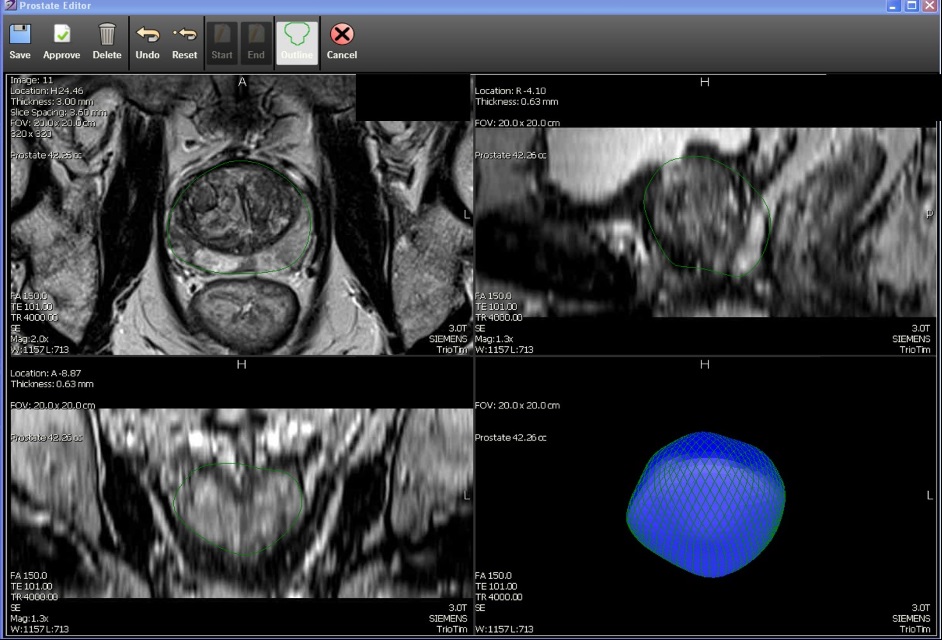
Post Processing
|
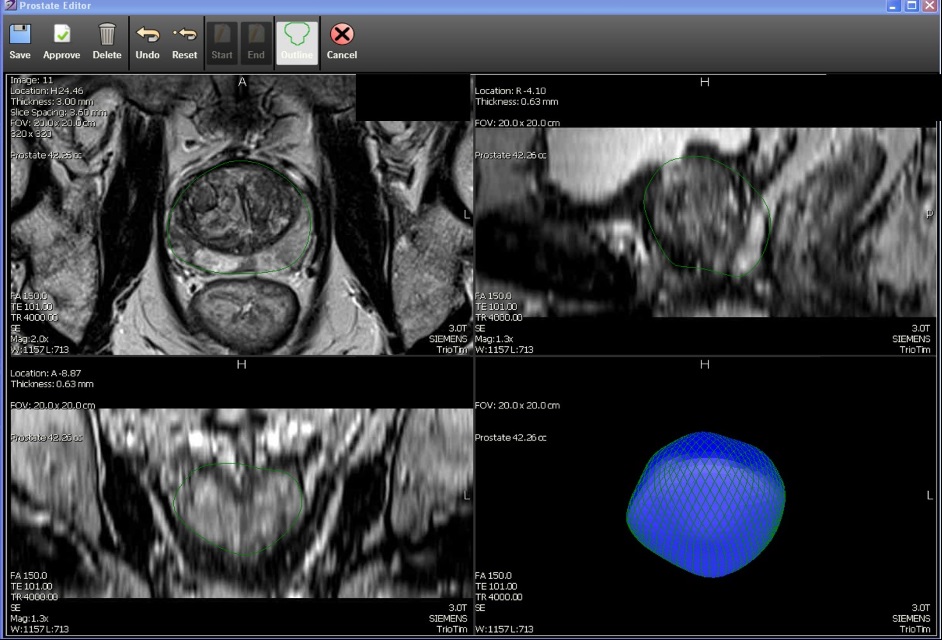
Gland segmentation and ROI-target lesion identification for UroNav MRI-US guided-fusion biopsy is performed using commercially available software (DynaCad, Invivo, Gainesville, FL). DynaCad has semi-automated gland segmentation and user specified ROI-targeting.
|